Shoulder Arthroplasty
ANATOMY

SYMPTOMS
In the past months to years, the mobility of your shoulder has deterio-rated considerably. Many arm movements are associated with pain, and you are increasingly plagued by pain, even at night. Anti-inflammatory pain medication gives you only a temporary relief.
EXAMINATION
The mobility of your shoulder is painfully restricted in all directions. Cer-tain movements can be associated with a noticeable (sometimes even audible) crunch. If certain movements are no longer possible due to the lack of force, there may also be a defect in the tendons arranged around the head of the humerus (rotator cuff).
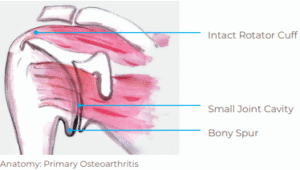
The narrowed joint cavity can be seen in the x-ray as a sign of cartilage wear. Often there are also bony spikes (osteophytes) and changes in the original joint shape.
For a more precise assessment of the osteoarthritis and the condition of the surrounding soft tissue, an MRI (magnetic resonance imaging) or a CT examination (computed tomography) is usually carried out.

For a more precise assessment of the osteoarthritis and the condition of the surrounding soft tissue, an MRI (magnetic resonance imaging) or a CT examination (computed tomography) is usually carried out.

TREATMENT AND OPERATION
Usually non-operative treatment including physiotherapy, anti-inflammatory painkillers and possibly also a steroid injection into the affected joint are initiated first. However, if your complaints persist and after careful assessment, we may recommend to perform a total shoulder arthroplasty. There are two fundamentally different options.
Anatomic Shoulder Arthroplasty
In primary osteoarthritis with cartilage destruction, we opt for the so-called anatomical shoulder arthroplasty, which mimics the original joint as closely as possible and therefore relies on an intact rotator cuff.
Reverse Shoulder Arthroplasty
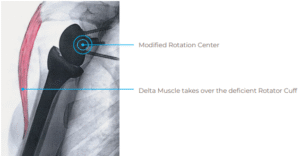
If, on the other hand, there is an extensive rotator cuff insufficiency, a so called rotator cuff arthropathy, the anatomic arthroplasty men-tioned above does not provide sufficient joint guidance and therefore only results in poor function of the joint.

X-ray: Osteoarthritis with irreparable rotator cuff defect
In these cases, we opt for the so-called reverse shoulder arthroplasty. “Reverse” because a hemisphere is used in the area of the former joint socket and a socket in the area of the humerus. This leads to a more stable joint movement. In addition, the shifting of the fulcrum enables the deltoid muscle to at least partially raise the arm despite the insuffi-cient rotator cuff. Although this is of great benefit for many patients, we would like to point out that the deltoid muscle may not bring back all previously missing movements in this technique.
AIM
With both types of arthroplasty, our main goal is to relieve you of pain as much as possible. Furthermore, it is not always possible to improve mobility and strength. This is due to the fact that the shoulder joint is more dependent on the good functioning of the surrounding soft tis-sues and muscles than other joints and that these have often been “out of order” for a long time with osteoarthritis. Therefore, we cannot expect them to automatically resume their function after the joint has been replaced. Depending on the initial situation, a partial restriction of mobility can remain even after a successful operation.
RISK
You are treated by experienced surgeons. However, no intervention is free from risks or possible complications. The main risks are:
- Joint infection 1.8%
- Injury to large blood vessels 0.5 – 1%
- Injury to large nerves 0.5 – 1%
- Painful loosening of a prosthetic component: after 10 years 5 – 15% (depending on the type of arthroplasty and strain)
- Dislocation of the joint ~ 3-5% with the reverse prosthesis ~ 1% for the anatomical prosthesis
- Later functional deterioration due to later injuries to the soft tissue
HOSPITAL STAY
Your arm will be immobilized on an abduction pillow for the first six weeks after the operation. Nevertheless, from the first day onwards you will take up passive and supported movement exercises with our physiotherapists and carry them out independently. The hospital stay will last about 3-4 nights.
DISCHARGE
The physiotherapy will continue seamlessly after your discharge. This takes place usually on an outpatient basis, rarely as part of an inpatient stay in a rehabilitation clinic, if needed due to your health status and costs are covered by your insurance. The suture material is removed after about 12 days by your family doctor or in the rehabilitation clinic. The abduction pillow may be omitted after the first consultation in our clinic six weeks after the operation. Movement therapy is also continu-ously increased. It is usually possible to drive a car for short distances after about 8-10 weeks.
After about 3 months, you will be able to strain your arm with moder-ate strength in everyday life. However, physical therapy to improve mobility and strength will continue for about six months after the pro-cedure.
QUESTIONNAIRE: QUALITY CONTROL
All patients operated on the shoulder in our clinic are asked to fill out a questionnaire. This questionnaire includes questions about discom-forts and the functionality of everyday life. With this, we gain valuable information about your treatment process. You will receive this ques-tionnaire before the operation, 6, 12, and 24 months after the opera-tion. Participation in this project is of course voluntary and does not affect your therapy.