- Home
- The Orthobiological Possibilities for Knee-Preservative Therapy Meniscus Replacement Cartilage Treatment
The Orthobiological Possibilities for Knee-Preservative Therapy Meniscus Replacement Cartilage Treatment
BASICS
If the meniscus and cartilage are injured, they can be reconstructed! Innovative methods exist by which it is possible to repair missing cartilage structures (meniscus, articular cartilage) with complex replacement materials. This opens up completely new possibilities for you. However, it is important to understand something in advance: What is common to all of these biological replacement methods is that the operation itself is only a small part of the overall treatment concept. Follow-up treatment in the months after the operation requires patience and commitment on your part, typically around one year.
If you are ready to take on this crucial phase after the operation, there is a good chance that your knee joint will be less painful and more resilient in a year, in comparison to now. Deliberately, we have not listed the implant options. The basis for cartilage material replacement is always: a well-balanced leg axis (no strong bow or X leg), and a ligament-stable joint. If these requirements are not met, they would still have to be created, either simultaneously or in advance of the cartilage replacement operation (see also Fig. 9/10).
LEGEND
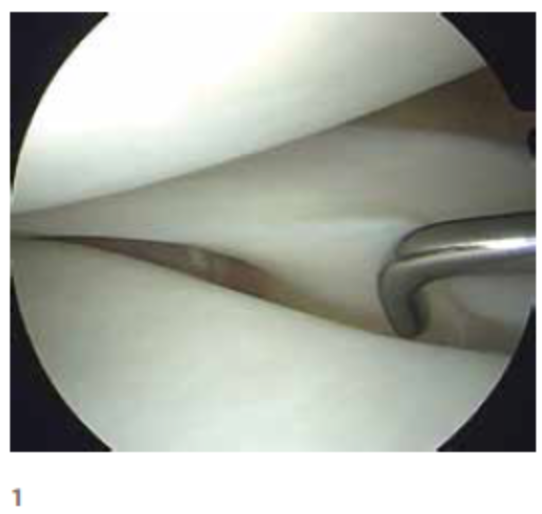
Arthroscopic images of a right knee.
1 – Normal meniscus 2 After partial meniscus removal
2 – After partial meniscus removal
3 – Healthy cartilage
4 – Cartilage damage
PATIENT SPECIFIC TREATMENT
In order to be able to professionally treat your problem, we differentiate between arthroscopic procedures and operations in which your joint is opened. Depending on the location, as well as the size and depth of the defect, we can recommend the following options:
Micro-Fracture Treatment
Our experience since 1999: This is an arthroscopic procedure. It can be used to treat a cartilage damaged zone of up to approximately 2 cm2. The damage is first cleaned up, down to the bone. The damage is cleaned at the edges, so that the cartilage in the edge zone is firmly connected to the underlying bone. Then, using awl-like instruments, small holes are made through the hard bone layer. This releases stem cells from the bone marrow. Within a few weeks, from this bone marrow blood clot, a new layer of scar (replacement) cartilage is formed.
Cell-Free Cartilage Replacement Material
e.g. CaReS-1S or BST-Cargel: Our experience since 2004: This is an open surgical procedure. Your cartilage damage is larger than 2 cm2 or the results of the micro-fracture technique have been disappointing. Thus, something else is required. Damaged cartilage is removed down to the bone (debridement) except for stable surrounding cartilage. In the now available defect zone, we glue a gel-like product that consists of collagen. Your cartilage cells from the surrounding area will migrate into this cell-free tissue and finally, after several months build up a joint-like layer again.
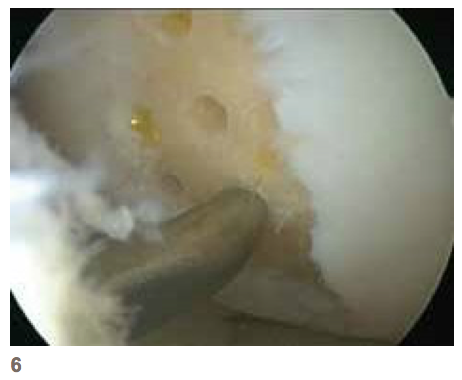
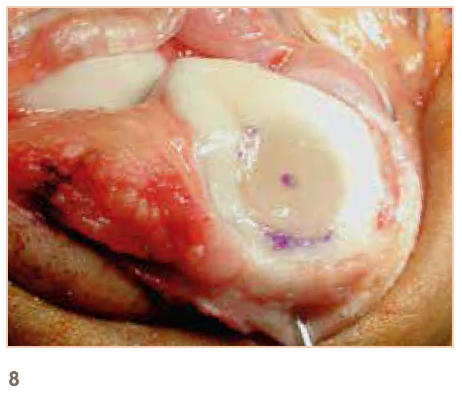
LEGEND
5 – Cartilage damage before treatment
6 – After arthroscopic micro-fracture
7 – Kneecap with cartilage damage after debridement
8 – Replacement with CaReS-1S
Cartilage/Bone Replacement (Osteotendonal Reconstruction).
e.g. MaioRegen: Our experience since 2011: If, in addition to the cartilage, the under- lying bone is also damaged, we treat this very crucial zone as well. In an open procedure, we remove the damaged cartilage and modified bone. We press the replace-ment material, especially produced for this, into the gap. It is cell free but enables the cartilage cells in the respective layer to form cartilage like tissue and the bone cells to build up bone again.
 Cartilage Cell/Autologous Cartilage Transpantation (ACT)
Cartilage Cell/Autologous Cartilage Transpantation (ACT)
Our experience since 2003: Good studies have shown that cartilage cell transplantation is currently the best solution for repair tissue quality and longterm results. We can confirm this experience, especially when there is large cartilage damage. In a first small arthroscopy, cartilage cells are removed. These are grown in the laboratory. Three weeks later, a patch of your own cells can be used in an open operation. This obviously requires a lot of effort, technologi-cally and operationally, as well as on your part in the phase after the operation.
LEGEND
9 – Inside right knee joint with large bone cartilage defect
10 – Inside right knee joint with a MaioRegen replacement
11 – Large oval cartilage defect on the back of the kneecap
12 – Back of the kneecap with inserted ACT material
Partial-Meniscus Implant
e.g. ActiFit: Our experience since 2009. You had to remove a large part of a meniscus after it was damaged. Your knee joint does not tolerate this and is painful under load. A replacement product made of high-tech polyurethane can help you. In an arthroscopic operation, we remove the unstable portions of the meniscus and ensure that the docking area on the remaining meniscus is well supplied with blood. The sides of the meniscus must still be intact and available to be used. We arthroscopically suture the artificial meniscus onto these. Within a few months, the artificial material will be colonized by your own cells and converted into a meniscus-like tissue. The artificial material will slowly be broken down, your body’s own tissue will take over the function.

LEGEND
12 – Arthroscopic images of the right knee joint
13 – Inner meniscus after subtotal removal
14 – ActiFit inner meniscus-replacement
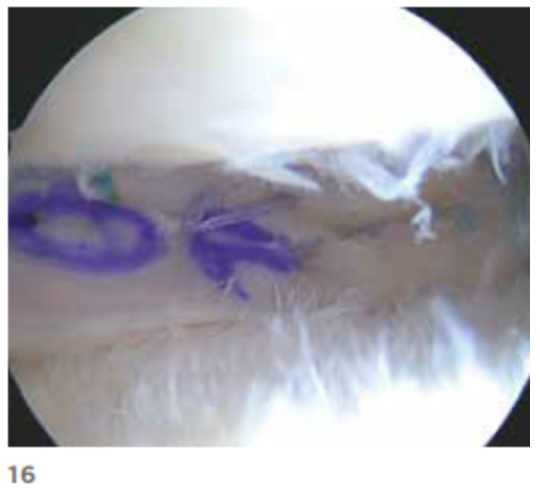
Allograft Meniscal Transplant
Our experience since 2011: The whole meniscus is gone, in any case the edge has been torn through, and you have complaints. You can be helped with insertion of an Allograft meniscus. A donor meniscus corresponding to your measurements is ordered and implanted arthroscopically. Rejection reactions rarely occur since your donated meniscus is of course delivered sterile, but alsocell free. This procedure is particularly useful for the external meniscus. Logistically, some of these treatment options are quite demanding. In particular, the issue of cost reimbursement from your insurance company can extend the phase from the decision for treatment to the actual operation.
LEGEND
15 – Arthroscopic images of the right knee
16 – After total loss of the external meniscus
17 – After using a donor meniscus
Donor meniscus before use
RISKS
Any procedure, which is supposed to improve the resilience and durability of your knee joint, using biological methods, can also have the opposite effect. Experience shows that around 85 – 90% of the patients treated in this way can expect a significant improvement in their quality of life. Experienced surgeons treat you and we have several years of experience with the procedures mentioned. Still, it’s like flying – no surgery is without risk. The risks of this operation can be summarized as follows:
- Risk of infection: ~ 1%
- Likelihood that you will require a blood transfusion: ~ 0%
- Damage to relevant vessels: less than 1%
- Damage to relevant nerves: less than 1%
- Thrombosis/Embolism: ~ 1%
- Failure of the implant; no relevant improvement after 12 months: 10 – 15%
HOSPITAL STAY
After an orthobiological reconstruction of your knee joint, you will stay in the hospital for between 2 and 4 nights, depending on the operation. The day after the operation, the drain (if used) will be removed from your knee, on the second day the swelling and the wound will be checked. All procedures are common in that the knee joint should not be weight-bearing. You may walk on crutches with no more than a 10 kg partial load for 6 weeks. After cartilage replacement surgery, a Kinetec splint will be delivered to your home. After replacement of the meniscus, a special knee brace to limit your freedom of flexion in the knee joint to 90 ° will be used. Sometimes this is also necessary when replacing cartilage behind the kneecap.
DISCHARGE
You will go home when you are practically pain-free, moving well with crutches, and feeling comfortable with your knee and the entire situation. You will be discharged with a prescription for physiotherapy, the necessary medication for swelling, pain relief and thrombosis prophylaxis as well as a check-up date with us. Your family doctor will remove the stitches about 10 – 14 days after the operation. We will see you in our out-patient clinic for your first check-up, after 6 weeks.
pdf for download: Orthobiological Possibilities