- Home
- Hallux valgus
Hallux valgus
DEFINITION/FORMATION
The hallux valgus or bunion is probably the most common foot problem. How this deformity emerges is not entirely clear. A genetic predisposition and tight shoes worn for years are considered a partial cause of the change.
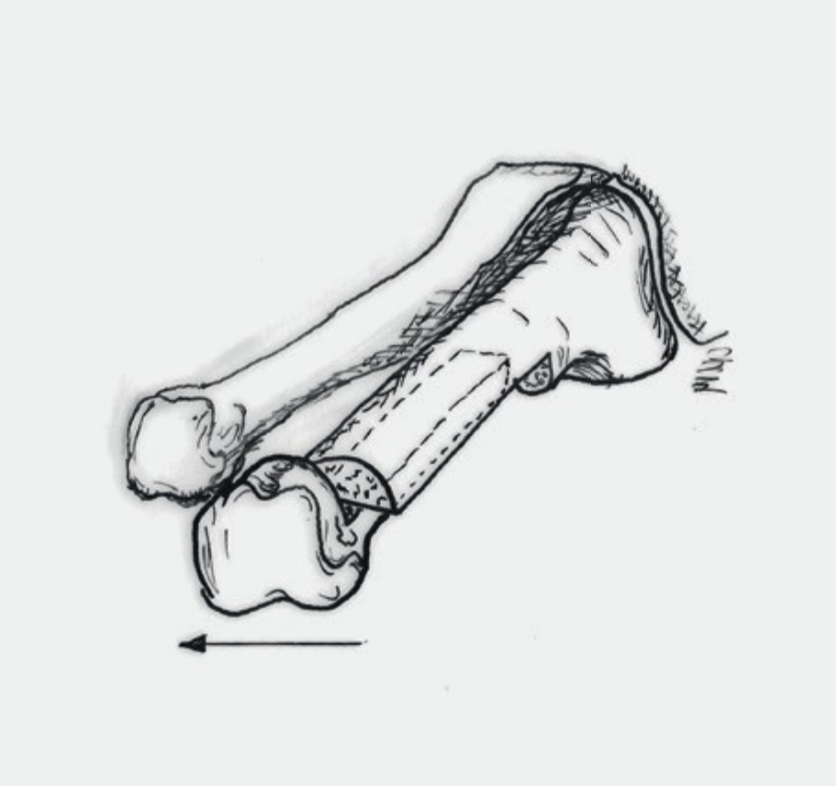
The deformity is characterized by the big toe tilting outward while the metatarsal bone deviates inwards (Fig. 1). A mostly painful bunion is seen above the base joint. However, this is not an additional bone, but the head of the first metatarsal. The pressure from the shoes becomes painful and often leads to the formation of a small bursa over the head of the first metatarsal, which causes additional pain. The feeling of numbness or burning of the big toe, which is also very uncomfortable, is caused by the irritation of a skin nerve that runs over the bulging head.
Due to the lateral deviation, the big toe loses its support function for the arch of the foot. The pressure on the sole of the foot while standing and walking is transferred to the neighboring metatarsals. This often results in painful overload and calluses under the heads of the second and third metatarsals. This overload, in turn, often weakens the joints of the second and third toes. The result is hammer toes (Fig. 2). This explains the very common combination of hallux valgus and hammer toe deformity.
SYMPTOMS
Most patients notice a deformity. Redness is often formed over the bunion. It is also possible to have signs of pressure marks or even skin injuries from the worn shoes. Occasional pain can occur, but it is quite diverse and has no direct connection with the extent of the deformity. It could be that the strongest deformity may cause no pain at all, while even minor deformities can trigger severe pain.

EXAMINATION
The deformity of the toes is noticeable during the examination. It is important to assess this misalignment while standing, i.e. with the foot under pressure. Possible redness, bruises or corns may be visible and changes in the pattern of calluses on the sole of the foot may appear. The x-ray image shows the extent of the deviation of the first metatarsal inwards (Fig. 3).
TREATMENT
The hallux valgus is not a dangerous transformation. Only the pain and the restricted mobility and thus the patient himself can determine whether an operation is necessary. In the event of minor complaints or purely cosmetic changes, we do not recommend the surgery. The extent of the deformity alone is not a reason to have the operation. If an initially pain-free deformity increases over time and causes more problems, surgical correction is still possible and justified.
A) Non Surgical
Conservative treatments cannot reverse the deformity, but occasionally they can help reduce the symptoms. There are various aids such as toe spacers, splints etc. that can be tried out. Sometimes it also makes sense to have insoles made, as well as wearing appropriate footwear to avoid pressure marks.
B) Surgical
There are a variety of surgical techniques to correct a hallux valgus. The common goal of all of the procedures is the most exact possible restoration of the normal anatomy as it was before the deformity. The tilted metatarsal bone is straightened up and stabilized. This allows the big toe to be brought into a correct position and restores its support function. The painful pressure points on the sole of the foot are therefore usually relieved.
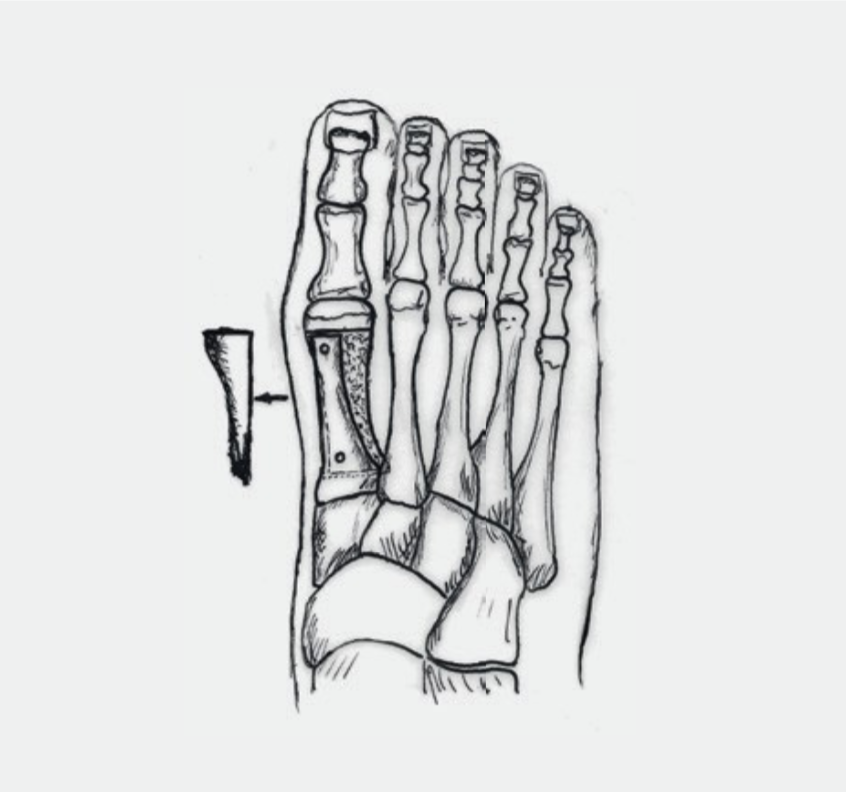
1. Osteotomy: Our most common used technique is the SCARF-Osteotomy (Fig.4). The required correction can be achieved with a bone cut (osteotomy). The severed bones are held in place by two small screws until they are stable and healed (six to eight weeks). Alternatively, the CHEVRON osteotomy, where only one screw is inserted, is occasionally used for slight deformity. The screws have no function after 3–4 months and are usually left as they do not interfere and are biologically harmless. In the first 6 weeks after the operation, the foot in the forefoot relief shoe (Fig. 7a) may be weight beared at the heel according to the discomforts.
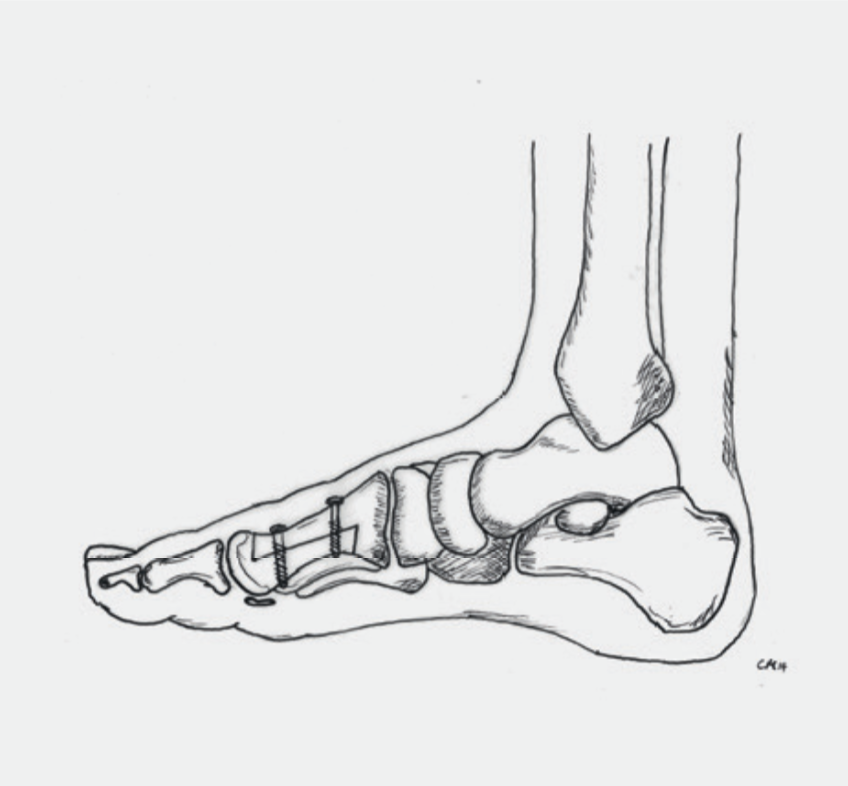
Fusion: In the case of a pronounced malposition of the big toe and/or the first metatarsal, but even with additional changes in the joints, other corrective techniques are sometimes used. This includes the fusion (arthrodesis) of the big toe’s base joint (Fig. 5) or the first metatarsal joint (Fig. 6). In the first 6 weeks after the operation, the foot is in the VACOpedes (Fig. 7b) and may only be partially weight beared. These techniques also have the goal to achieve pain-free walking again.


RISKS AND COMPLICATIONS
Complications and risks can occur during or after the operation, delaying the healing process or requiring another operation. Even though they are rare for foot operations, they can never be completely ruled out.
In summary, these are:
- Healing disorders
- Infections
- Vascular injuries, post-operative bleeding, hematoma, blood loss
- Nerve injury
- Non Union (lack of bone healing)
- Fracture
- Bothering Implants (screws, plates)
- Thrombosis, embolism
- Residual symptoms
- Renewed deformity
Unfortunately, the hallux valgus surgery has a bad reputation as being a very painful and unsuccessful procedure. Many patients know of relevant reports from their own circle of friends.
The fact is that the correction of the hallux valgus deformity is a very demanding surgery and requires a lot of experience. In expert hands, it is one of the most successful operations in foot surgery.
FOLLOW-UP TREATMENT
The surgery is only a part of the whole treatment. Follow-up treatment contributes significantly to its success. It is important that you know what you should be aware of and what you should possibly avoid.
Dressing and Wound Care
During the time in the hospital you will be shown how to take care of the wound. As long as the wound is not completely dry (wound secretions/blood), the dressing should be changed daily. Do not apply any ointments or powder directly to the surface of the wound until the stitches have been removed! Disinfection is not necessary. Always remove the entire dressing when changing. The new dressing must be dry and must not slip.
Once the wound is dry, a normal plaster (quick bandage) is sufficient. An elastic bandage can protect and cushion the operated area. This will also reduce the swelling that is still present. If you are not sure whether everything is normal, you can contact your family doctor or contact us directly.
The stitches can be removed about 2 weeks after the operation, this is usually done by the family doctor.
Swelling and Pain
After an operation, the affected foot is always more or less swollen. This swelling can recur for weeks (for up to 6 months). The most effective measure to prevent this is to elevate the leg. At home, the foot should be elevated often during the first few weeks. It also makes sense to move several times a day (walking, not as much standing) but only for a short time. It is time to elevate the leg if the foot is tense and starts to hurt again.
It is important to know that the foot generally tends to swell after foot operations. This reaction is normal and disappears after 6 to 12 months.
Pain in the operated foot can occur in the first few days and weeks after the operation despite these measures. However, to relieve the pain, you can take the pain medication prescribed to you.
Weight Bearing
The permitted weight bearing of the foot depends on the operation performed. You received a special shoe to protect and to simplify your mobility (Fig.7). Depending on the operation, either partial weight bearing was recommended, or full weight bearing was allowed. In the beginning, getting up should be kept to a minimum. There is a strong tendency for the foot to swell. Bleeding can occur as well in the wound area due to standing and walking for long periods.
Full Weight Bearing
As soon as the pain allows it, you may fully weight bear the foot. It is important that the special shoe is worn consistently throughout the first 6 weeks. The crutches are mainly used for security reasons and can slowly be omitted.
Partial Weight Bearing
You may put about 25 kg of weight on the affected foot. This roughly corresponds with the weight of the leg and means that you always have to use crutches. Our physiotherapists will instruct you accordingly in order to be able to implement this correctly. It is important that you can use the stairs with the aid of crutches by yourself. It is also critical that the special shoe is worn consistently, and the crutches are used for the first 6 weeks.
Personal Hygiene
As long as the stitches are still in the wound, i.e. usually in the first 2 weeks, the operated foot should be protected with a plastic bag. The easiest way is to pull the plastic bag over the special shoe. As soon as the stitches are removed, you can shower and bathe without further precautionary measures.
Thrombosis Prophylaxis
Thrombosis prophylaxis begins during the hospital stay. Depending on the operation, this prophylaxis must be continued. In most cases, we use Fragmin 5000IE pre-filled syringes, which are injected by the patient themselves once a day. You will be instructed by our nursing staff during your stay.
How long you need the injections depends on the operation, the individual risks and is necessary until you can fully weight bear your foot and walk without crutches again, in about 6-8 weeks.
Work Ability
A rest period is crucial after an operation. In the first 2 weeks you should take care of yourself and not work. How long you will be unfit for work depends on the type of surgery as well as your stress profile. In most cases you and your employer should be able to temporarily find less stressful work. This enables early resumption of work.
The signed work absence that you will receive from us is a preliminary assessment. The certificate can be extended if you are not able to resume work after this time. If this is the case, report to your family doctor or to us.
However, you may take up your work again any time before the given date, if you feel capable to do so.
Driving a Car
At what point you can resume driving again depends on the kind of operation you had. You must refrain from driving as long as you cannot fully weight bear your foot or are still requiring crutches. How far thereafter your ability to drive is restored is up to you. In case of doubt or if you are unsure, we recommend avoiding driving.
Check-Ups
Your surgeon will require x-rays to be taken 6 weeks after the operation. The further procedure will then be determined. In most cases you will be able to wear your own shoes from then on. We recommend starting with shoes with a firm sole and soft upper leather.
Most activities can be resumed about 3 months after the operation. Sports activities should be increased slowly as not to provoke an overuse after a longer sport break.
pdf for download: Hallux Valgus