- Home
- Achillodynia and Haglund Exostosis Treatment
Achillodynia and Haglund Exostosis Treatment
DEFINITION/DEVELOPMENT
Like many tendons in the body, the Achilles tendon can also cause pain due to degenerative changes. Repetitive or unusually heavy strain can occasionally be found as a cause. Overweight or additional malpositioning of the foot are also considered to be triggers for such degenerative changes. In most cases, however, no actual trigger can be identified.

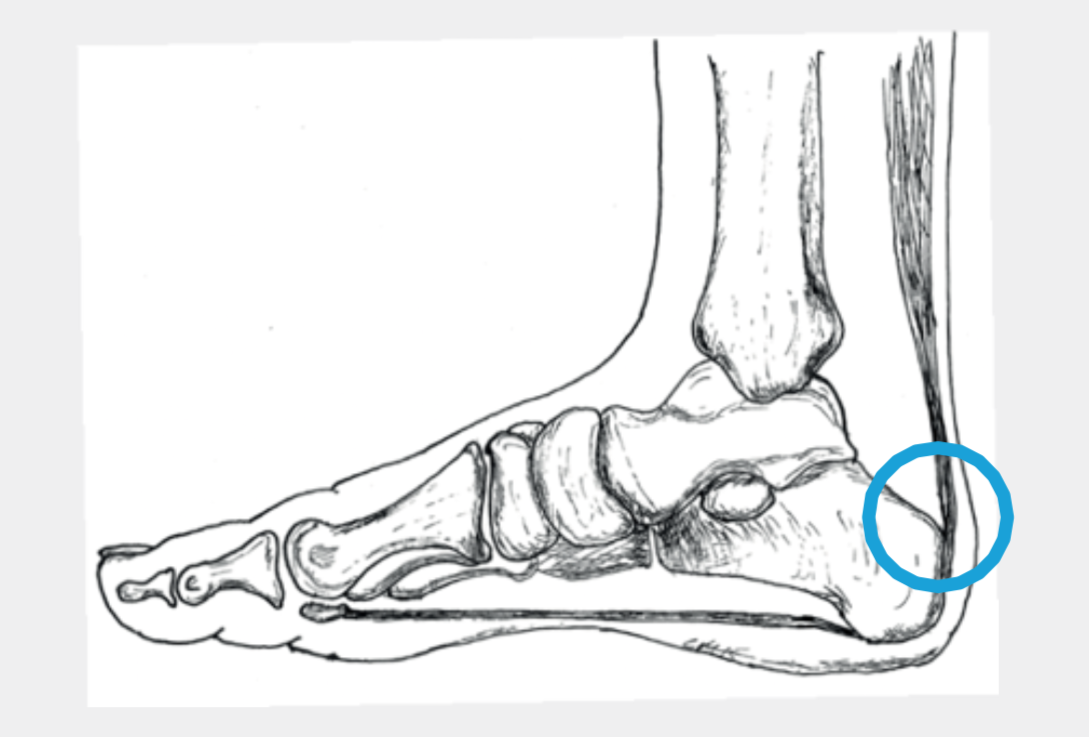
Typically, in achillodynia, the degeneration is found about 6 cm above the heel bone. At this height, the blood supply to the tendon is less than at other locations due to anatomical conditions. The spindle-shaped, usually painful swelling in this area is striking (Fig. 1). The second most common area affected is the Achilles tendon insertion. In addition to the degenerative changes, calcifications and spur formations can also occur here (Fig. 2).


Certain patients have a very prominent heel bone protrusion at the rear outside, called Haglund exostosis (Fig. 3). Occasionally, this “excess leg” causes complaints, especially in hard, closed shoes.
SYMPTOMS
Achillodynia regularly causes pain under stress. The first steps after getting up in the morning are often very painful but the pain decreases in the course of the first hour, only to increase again in the course of the day.
Pain at the base of the Achilles tendon is also usually load-dependent. This is possibly compounded by problems when wearing hard, closed shoes. Haglund exostosis primarily leads to pressure problems in footwear.
EXAMINATION
The examination reveals prominent bone protrusions. In addition to the shape of the foot, the length of the Achilles tendon is assessed, especially when the knee is stretched. There is often a slight shortening of the muscles and tendon. To determine the further procedure, an MRI may be useful for achillodynia and Achilles tendon insertion complaints. This allows the exact extent of the degeneration to be determined and the risk of a possible tear of the tendon to be estimated. Partial tears of the tendon can occasionally be detected which cannot be identified by a clinical examination.

TREATMENT
A) Non Surgical
Physiotherapy: If there is no risk of a tear and no treatment has been performed yet, a non surgical treatment should be chosen. Here, special attention is paid that the stretching of the muscles and the chronic inflammation of the tissue around the tendon is treated locally. The tendon can be specifically strengthened by eccentric strengthening (braking power). In addition, a soft insole can be placed under the heel or a special bandage can be worn (Fig.4).
PRP-Infiltration: PRP (platelet rich plasma) is obtained from the blood by centrifugation and contains a high concentration of platelets and growth factors. These growth factors are important in the healing processes and also appear to have a positive effect on tendon changes. The PRP is obtained from the blood of the affected patient, i.e. it is the body’s own growth factor, which is brought directly to the altered tendon parts in higher concentrations. Since the positive effect in the area of the Achilles tendon has not been scientifically proven, however, the health insurance does not cover the costs.
Shock wave therapy: Shock waves are sound waves that cause irritation and thus lead to increased blood flow to the altered tendon tissue. This promotes the healing process and can sometimes even lead to a dissolution of calcium deposits.
B) Surgical
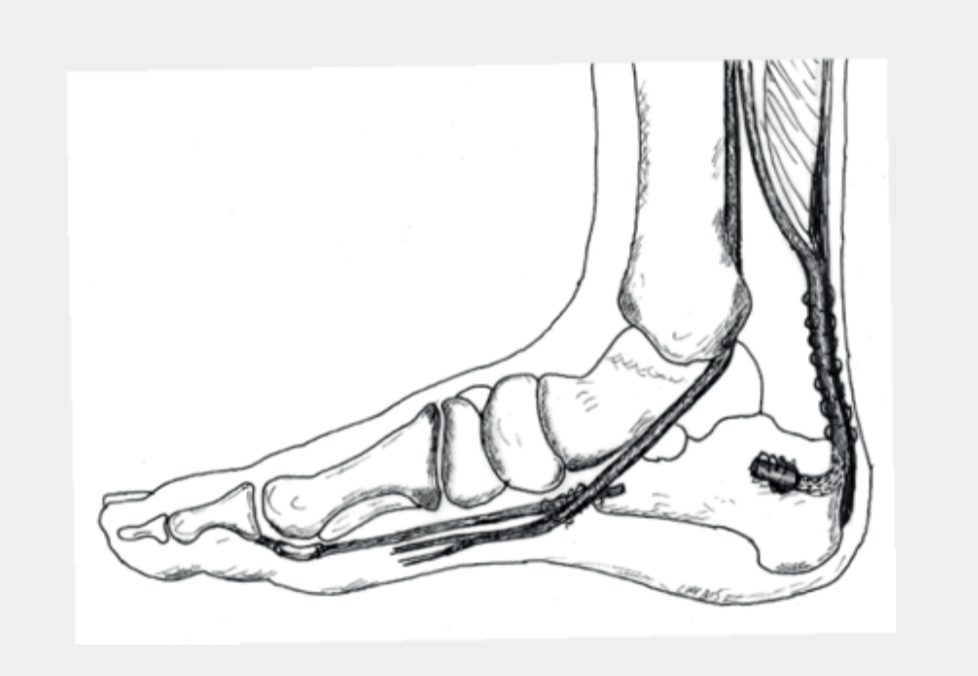
If there is no improvement after three to six months, an operative procedure may be advisable. First of all, the changed areas are cut out. If the tendon attachment is affected, calcifications and bone spurs are removed. Depending on the amount of the remaining tendon, it may have to be additionally strengthened by the body’s own tendon (tendon transfer, Fig.5).
Various surgical techniques are used here. The long flexor tendon of the big toe is used most frequently. Due to existing connections to the other flexor tendon, you can still bend the big toe after such an operation. The force is slightly reduced, but this is not relevant for everyday activities. At most young, very athletic patients occasionally notice a difference. Follow-up treatment must be individually coordinated in each case. However, immobilization in a VACOped (Fig.8) for several weeks is always necessary.
IMPORTANT: Rehabilitation after Achilles tendon surgery is lengthy, it can take up to 2 years!
Haglund exostosis: If suitable footwear and stretching of any shortening in the calf muscles does not lead to an improvement in symptoms, a Haglund exostosis can be surgically removed (Fig 6.). Follow-up treatment also consists of immobilization in a VACOped (Fig.8), but usually for less time than with the surgery of the tendon itself. The loss of work and sports break are shorter.
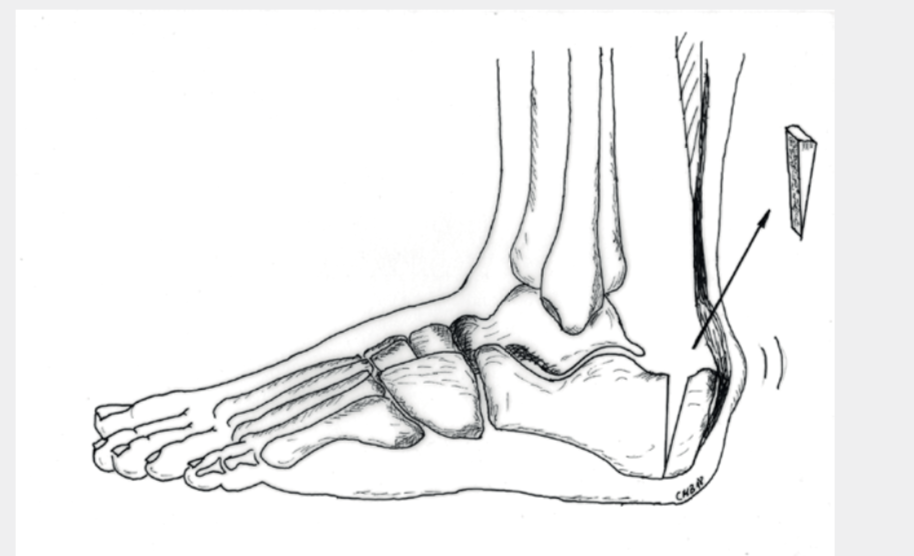
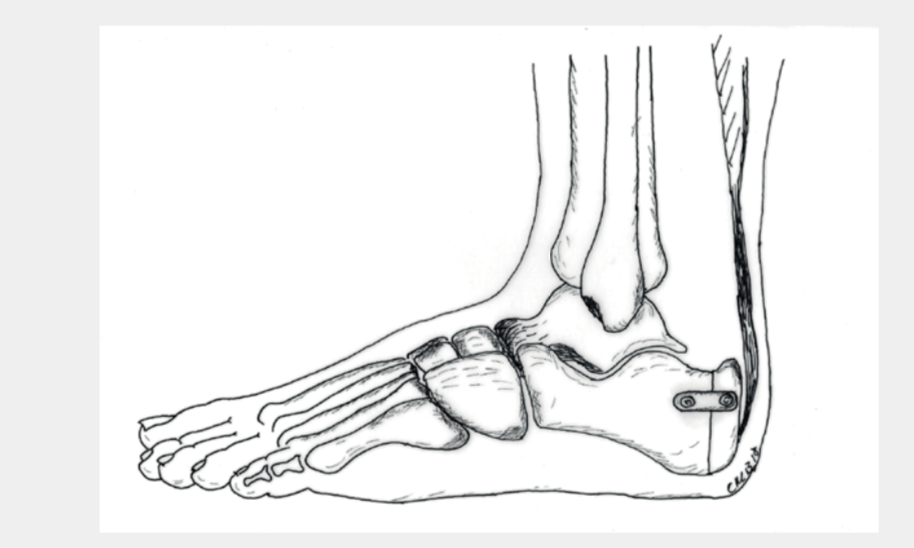
Kelly Keck Osteotomy: In certain situations, there is the possibility of indirect removal of the bone spurs with simultaneous slight relief of the Achilles tendon without surgery on the tendon itself. This is usually associated with an overall somewhat shorter rehabilitation phase. A wedge is removed from the heel bone from the outside (Fig.7a) and the bone is then reattached with a clasp, plate and/or screws (Fig.7b). Follow-up treatment involves immobilization in a VACOped (Fig.8) and partial weight bearing for 6 weeks. Afterwards, the load can be increased relatively quickly.
RISKS AND COMPLICATIONS
Complications and risks may occur during or after the operation and delay the healing process or make further surgery necessary. They can never be completely ruled out during an operation, even if they are rare during foot surgery. These are summarized below:
- Wound healing disorders
- Infections
- Vascular injuries, post-operative bleeding, hematoma, blood loss – Nerve injury
- Thrombosis, embolism
- Residual complaints
FOLLOW-UP TREATMENT
The surgery is only a part of the whole treatment. Follow-up treatment contributes significantly to success. It is important that you know what you should consider and possibly avoid.
The functional aftercare begins the day after the operation. With a special boot (VACOped, Fig.8) the patient can be mobilized again. Depending on the situation during the operation, you may put more or less weight bearing on the foot. Occasionally, starting from a pointed foot position, the position is back to normal in 6 weeks (3 weeks 30°, then 3 weeks 15°).

Dressing and Wound Care
During the time in the hospital you will be shown how to care for the wound. As long as the wound is not completely dry (wound secretion/blood), the dressing should be changed daily. Do not use ointments or powders directly on the wound surface as long as the stitches have not been removed! Disinfection is not necessary. Always remove the entire dressing when changing. The new dressing must be dry and must not slip. If the wound is dry, a normal plaster (quick bandage) is sufficient. An elastic bandage can protect and cushion the operated area a little. The remaining swelling is also reduced. If you are not sure whether everything is normal, you can consult your family doctor or contact us directly. The stitches can be removed about 2 weeks after the operation, this is usually done by your family doctor.
Swelling and Pain
After an operation, the affected leg is always more or less swollen. This swelling can recur for weeks (up to 6 months). The most effective measure to prevent this is to elevate the leg. It also makes sense to move several times a day (walking, less standing) but only for a short time. It is time to elevate the leg again if the foot/calf is tense and starts to hurt again.
Pain in the operated foot can occur in the first few days and weeks after the operation despite these measures. However, to relieve the pain, you can take the prescribed pain medication.
Weight-Bearing
The permitted weight bearing of the foot depends on the operation performed. You received a VACOped (Fig.8) to protect and simplify mobility. Depending on the operation, partial weight-bearing was permitted, or full weight-bearing was allowed. During the first 2 weeks, partial weight-bearing is nevertheless recommended until the wound has healed.
Partial Weight-Bearing
You are allowed to put about 25 kg of weight on the affected foot. This roughly corresponds to the weight of the leg and means that you always have to use crutches. Our physiotherapists will instruct you accordingly in order to be able to implement this correctly. It is important that you can use the stairs with the aid of crutches by yourself.
Full Weight-Bearing
As soon as the pain allows it, you may put full weight-bearing on the foot. It is important that the special shoe is worn consistently through the first 6 weeks. The crutches are mainly used for security reasons and can slowly be omitted.
Personal Hygiene
As long as the stitches are still in the wound, i.e. usually in the first 2 weeks, the operated foot should be protected with a plastic bag. The easiest way is to pull the plastic bag over the special shoe. As soon as the stitches are removed, you can shower and bathe without further precautionary measures.
Thrombosis Prophylaxis
Thrombosis prophylaxis begins during the hospital stay. Depending on the operation, this prophylaxis must be continued. In most cases, we use Fragmin 5000IE pre-filled syringes, which are injected by the patient themselves once a day. You will be instructed by our nursing staff during your stay.
How long you need these injections depends on the operation, the individual risks and is necessary until you can fully weight-bear your foot and walk without crutches again, in about 8 weeks.
Work Ability
A rest period is crucial after an operation. In the first 2 weeks you should take care of yourself and not work. How long you will be unfit for work depends on the type of surgery as well as your stress profile. In most cases you and your employer should be able to temporarily find less stressful work. This enables early resumption of work.
The signed work absence that you will receive from us is a preliminary assessment. The certificate can be extended if you are not able to resume work after this time. If this is the case, report to your family doctor or to us.
However, you may take up your work again any time before the given date, if you feel capable to do so.
Driving a Car
At what point you can resume driving again depends on the kind of operation you had. You must refrain from driving as long as you cannot fully weight bear your foot or are still requiring crutches. How far thereafter your ability to drive is restored is up to you. In case of doubt or if you are unsure, we recommend to avoid driving.
Check-Ups
Your surgeon will require a check-up six weeks after the operation. Then the further procedure will be determined. As a rule, the VACOped can then be slowly dismantled and crutches can slowly be omitted. Continuing physiotherapy is important. Most activities can be resumed about three months after the operation. In the follow-up consultation your physician or your physiotherapist can advise you as of when certain sports can be taken up again.
pdf for download: Achillodynia and Haglund Exostosis Treatment